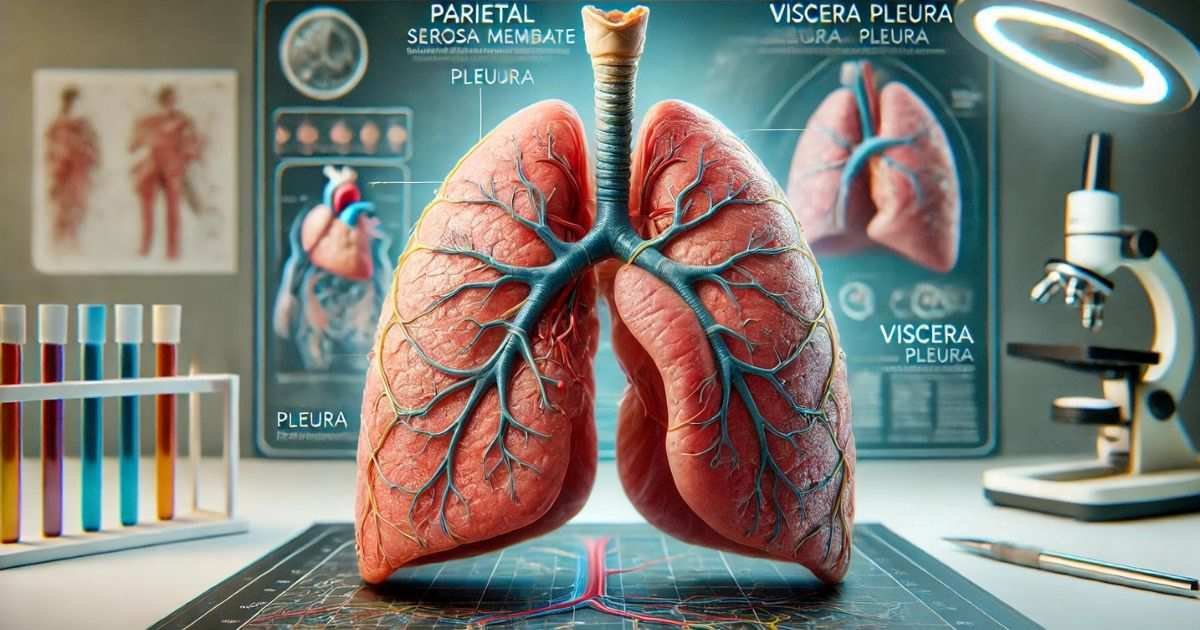
The inner serosa membrane that adheres to the lungs is a crucial component of the respiratory system. It is designed to facilitate the vital process of gas exchange, ensuring that oxygen reaches the bloodstream and carbon dioxide is expelled from the body. Central to this system are the lungs, which are not only delicate but also essential organs encased within the thoracic cavity. The pleura, a thin, double-layered membrane, plays a critical role in maintaining the functionality and protection of the lungs.
This membrane consists of the parietal pleura lining the chest wall and the visceral pleura adhering to the lung surface, with a pleural cavity filled with lubricating fluid in between. This structure is fundamental to the efficient and pain-free expansion and contraction of the lungs during respiration.
Understanding the pleura’s anatomy, function, and clinical significance is crucial for comprehending the overall respiratory mechanics and diagnosing various pleural diseases. Disorders involving the pleura, such as pleural effusion, pneumothorax, and pleurisy, can severely impact respiratory health and require timely medical intervention. Advances in diagnostic techniques and treatment methods continue to improve outcomes for patients with pleural conditions. This article provides a comprehensive examination of the inner serosa membrane, elucidating its essential role in respiratory physiology, the pathophysiology of pleural diseases, and the latest developments in pleural medicine.
Anatomy of the Pleura
Structure of the Pleura
The pleura is a critical anatomical structure that envelops the lungs and lines the interior of the thoracic cavity. This double-layered serous membrane is integral to the respiratory system’s functionality, providing both protection and a frictionless environment for lung movement. The pleura is divided into two main layers:
- Parietal Pleura: This outer layer adheres to the inner surface of the thoracic cavity, covering the diaphragm and the mediastinum. The parietal pleura is further divided based on its location: the costal pleura lines the rib cage, the diaphragmatic pleura covers the diaphragm, and the mediastinal pleura envelops the mediastinum. Each of these subdivisions plays a specific role in protecting and supporting the structures within the thoracic cavity.
- Visceral Pleura: The inner layer of the pleura, known as the visceral pleura, is intimately associated with the lung tissue itself. This layer closely follows the contours of the lungs, dipping into the fissures between the lobes. The visceral pleura is responsible for producing a serous fluid that fills the pleural cavity, ensuring the lungs can move smoothly against the thoracic wall during respiration.
Composition of the Pleura
The pleura is composed of specialized cells known as mesothelial cells, which are crucial for maintaining the serous environment within the pleural cavity. These cells secrete a small amount of lubricating fluid, known as pleural fluid, which significantly reduces friction between the pleural layers during respiratory movements. Beneath the mesothelial layer, the pleura contains several layers of connective tissue, which provide structural support and elasticity. These connective tissues include collagen and elastin fibers, which ensure the pleura can stretch and recoil as the lungs expand and contract.
Function of the Pleura
Protective Role
The pleura serves as a vital protective barrier for the lungs, safeguarding them from infections, physical injuries, and other potential threats. The serous fluid within the pleural cavity acts as a cushion, absorbing shocks and reducing mechanical stress during respiration and movement. Additionally, the pleura’s structure helps isolate the lungs from the rest of the thoracic cavity, minimizing the risk of infection spreading from adjacent organs or tissues.
Facilitating Lung Movement
One of the pleura’s most critical functions is facilitating the smooth movement of the lungs during the respiratory cycle. As the lungs expand and contract, the pleural fluid allows the visceral and parietal pleurae to glide effortlessly over each other. This lubrication is essential for minimizing friction and preventing damage to the delicate lung tissues and the thoracic wall. Without this fluid, the mechanical action of breathing would cause significant pain and potentially harmful frictional forces.
Maintaining Negative Pressure
The pleural cavity is maintained at a negative pressure relative to atmospheric pressure, a condition that is essential for proper lung inflation. This negative pressure ensures that the lungs remain expanded and adhere to the thoracic wall, even when not actively inhaling. During inhalation, the diaphragm and intercostal muscles expand the thoracic cavity, further reducing the pressure within the pleural cavity. This pressure difference allows air to flow into the lungs, facilitating efficient gas exchange. Maintaining this negative pressure is crucial for preventing lung collapse and ensuring consistent respiratory function.
Clinical Significance of the Pleura
Pleural Effusion
Pleural effusion refers to the accumulation of excess fluid within the pleural cavity. This condition can arise from various underlying causes, including infections (such as pneumonia or tuberculosis), malignancies (like lung cancer or mesothelioma), and systemic diseases (such as heart failure or liver cirrhosis). Symptoms of pleural effusion often include chest pain, shortness of breath, and a noticeable reduction in lung function. Diagnosis typically involves imaging studies such as chest X-rays, CT scans, or ultrasounds, which can visualize the fluid accumulation. Thoracentesis, a procedure where fluid is aspirated from the pleural cavity for analysis, is often performed to determine the underlying cause and guide appropriate treatment.
Pneumothorax
Pneumothorax occurs when air enters the pleural cavity, disrupting the negative pressure that normally keeps the lungs inflated. This condition can result from trauma, such as a rib fracture or penetrating injury, or spontaneously due to lung disease or certain medical procedures. The presence of air in the pleural cavity causes partial or complete lung collapse, leading to symptoms such as sudden chest pain, shortness of breath, and decreased breath sounds on the affected side. Treatment typically involves removing the air from the pleural cavity, often through the insertion of a chest tube, to allow the lung to re-expand and restore normal respiratory function.
Pleural Inflammation (Pleurisy)
Pleurisy, also known as pleuritis, is the inflammation of the pleura. This condition can result from infections (such as viral or bacterial pneumonia), autoimmune diseases (like rheumatoid arthritis or lupus), pulmonary embolism, or chest injuries. Pleurisy is characterized by sharp, stabbing chest pain that worsens with breathing, coughing, or sneezing. The inflamed pleurae rub against each other, causing significant discomfort and reducing respiratory efficiency.
Treatment for pleurisy focuses on addressing the underlying cause, such as administering antibiotics for infections or anti-inflammatory medications for autoimmune conditions. Pain relief is also a crucial component of managing pleurisy, often involving the use of analgesics or nonsteroidal anti-inflammatory drugs (NSAIDs).
The anatomy and function of the pleura are integral to the respiratory system’s overall health and efficiency. Understanding these aspects helps in diagnosing and treating various pleural disorders, ensuring better clinical outcomes and improved patient quality of life.
Pneumothorax
Pneumothorax occurs when air enters the pleural cavity, disrupting the negative pressure and causing lung collapse. This can result from trauma, lung disease, or spontaneously. Treatment involves the removal of air from the pleural cavity, often through a chest tube, to allow the lung to re-expand.
Pleural Inflammation (Pleurisy)
Pleurisy, or pleuritis, is the inflammation of the pleura, often due to infections, autoimmune diseases, or pulmonary embolism. It causes sharp chest pain that worsens with breathing. Treatment focuses on addressing the underlying cause and alleviating pain.
Diagnostic Techniques for Pleural Disorders
Diagnosing pleural disorders accurately is crucial for effective treatment and management. Several diagnostic techniques are employed to identify and assess conditions affecting the pleura. These include imaging studies, thoracentesis, and pleural biopsy. Each technique offers unique insights into pleural pathology and is often used in conjunction to provide a comprehensive evaluation.
Imaging Studies
Chest X-ray
Chest X-ray is one of the most commonly used diagnostic tools for detecting pleural abnormalities. It provides a quick and non-invasive way to visualize the pleural space and identify conditions such as pleural effusions, pneumothorax, and pleural thickening. In cases of pleural effusion, a chest X-ray can reveal the characteristic fluid levels, often seen as blunting of the costophrenic angles. Pneumothorax is identified by the presence of air in the pleural cavity, visible as an area devoid of lung markings. Chest X-rays are typically the first step in diagnosing pleural disorders and are essential for initial assessment and monitoring.
CT Scan
Computed Tomography (CT) scans offer a more detailed and precise imaging modality compared to chest X-rays. CT scans provide cross-sectional images of the chest, allowing for better visualization of pleural pathology, including subtle effusions, pleural masses, and complex pleural thickening. CT scans are particularly valuable in distinguishing between benign and malignant pleural diseases, assessing the extent of pleural involvement, and guiding interventional procedures. The high-resolution images obtained from CT scans help in the accurate localization of abnormalities and provide crucial information for planning further diagnostic or therapeutic interventions.
Ultrasound
Imaging Ultrasound is a versatile and non-invasive technique used to assess pleural effusions and guide procedures such as thoracentesis. Ultrasound is highly sensitive in detecting even small amounts of pleural fluid and can differentiate between simple and complex effusions based on the appearance of the fluid. Additionally, ultrasound can identify septations, loculated effusions, and pleural thickening. The real-time imaging capability of ultrasound makes it an invaluable tool for guiding needle placement during thoracentesis, ensuring safety and accuracy. Ultrasound-guided thoracentesis reduces the risk of complications and improves the diagnostic yield of the procedure.
Thoracentesis
Thoracentesis, also known as pleural tap, is a procedure where a needle is inserted into the pleural cavity to aspirate fluid for diagnostic or therapeutic purposes. This procedure is performed under local anesthesia and is often guided by ultrasound to ensure precise needle placement. Thoracentesis helps in diagnosing infections, malignancies, and other pleural conditions by providing a sample of pleural fluid for laboratory analysis. The aspirated fluid is subjected to various tests, including biochemical analysis, cytology, microbiological culture, and molecular studies.
These tests can identify the presence of infection, malignancy, or inflammatory conditions and provide critical information for determining the underlying cause of pleural effusion. Therapeutically, thoracentesis can relieve symptoms associated with large effusions, such as dyspnea and chest discomfort, by removing excess fluid from the pleural cavity.
Pleural Biopsy
A pleural biopsy involves taking a small sample of pleural tissue for histopathological examination. This procedure is indicated when pleural malignancies, tuberculosis, and other chronic pleural diseases need to be diagnosed that cannot be confirmed through fluid analysis alone. Different methods for obtaining a pleural biopsy exist, including needle biopsy, thoracoscopic biopsy, and open surgical biopsy.
Needle Biopsy
A less invasive method where a needle is used to obtain a tissue sample from the pleura. This can be performed under image guidance (such as CT or ultrasound) to improve accuracy. Needle biopsy is useful for diagnosing conditions like pleural tuberculosis and certain malignancies.
Thoracoscopic Biopsy
Video-assisted thoracoscopic Surgery (VATS) allows for direct visualization of the pleural surfaces and targeted biopsy of abnormal areas. This minimally invasive technique provides larger and more representative tissue samples, making it highly effective for diagnosing pleural malignancies and other complex pleural diseases. VATS is also beneficial for staging pleural cancer and assessing the extent of disease spread.
Open Surgical Biopsy
In cases where needle biopsy and thoracoscopic biopsy are inconclusive, an open surgical biopsy may be performed. This involves a thoracotomy, where a larger incision is made to access the pleural space and obtain a tissue sample. Open biopsy provides the most comprehensive and definitive diagnostic information but is more invasive and associated with a longer recovery time.
The histopathological examination of pleural biopsy samples can reveal the presence of malignant cells, granulomas, or other pathological changes that indicate specific diseases. This information is crucial for developing an appropriate treatment plan and predicting prognosis.
Accurate diagnosis of pleural disorders is essential for effective treatment and management. Imaging studies, thoracentesis, and pleural biopsy are key diagnostic techniques that provide valuable insights into pleural pathology. Combining these methods allows for a comprehensive evaluation, ensuring precise diagnosis and optimal patient care. Advances in imaging technology and minimally invasive procedures continue to improve diagnostic accuracy and patient outcomes in the field of pleural medicine.
Treatment and Management of Pleural Disorders
Effective treatment and management of pleural disorders require a multidisciplinary approach that combines medical management with surgical interventions when necessary. The choice of treatment depends on the underlying cause of the pleural condition, the severity of symptoms, and the overall health of the patient. Here, we discuss the various medical and surgical options available for managing pleural disorders.
Medical Management
Antibiotics
Antibiotics are the cornerstone of treatment for pleural effusions caused by bacterial infections. Common infectious causes include pneumonia, empyema, and tuberculosis. The choice of antibiotic depends on the suspected or confirmed pathogen, the patient’s clinical status, and local antibiotic resistance patterns. For example, broad-spectrum antibiotics may be initially prescribed to cover a wide range of bacteria until specific pathogens are identified through culture and sensitivity testing. Once the causative agent is known, the antibiotic regimen can be tailored accordingly to ensure effective eradication of the infection.
Anti-inflammatory Medications
Anti-inflammatory medications, including nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids, are used to reduce inflammation and alleviate pain in conditions such as pleurisy (pleuritis). NSAIDs, such as ibuprofen and naproxen, are commonly prescribed for their analgesic and anti-inflammatory effects. Corticosteroids, such as prednisone, may be used in more severe cases or when NSAIDs are contraindicated. These medications help reduce pleural inflammation, relieve chest pain, and improve respiratory function, allowing patients to breathe more comfortably.
Diuretics
Diuretics, such as furosemide (Lasix), are commonly used to manage pleural effusions secondary to heart failure. These medications help reduce fluid accumulation by promoting the excretion of excess fluid through the kidneys. By decreasing the volume of fluid in the pleural cavity, diuretics can relieve symptoms such as shortness of breath and improve overall lung function. It is essential to monitor electrolyte levels and kidney function regularly during diuretic therapy to prevent potential side effects.
Surgical Interventions
Chest Tube Insertion
Chest tube insertion, also known as thoracostomy, is a procedure used to drain large pleural effusions or air in the pleural cavity (pneumothorax). During the procedure, a flexible tube is inserted through the chest wall into the pleural space under local anesthesia or sedation. The tube is then connected to a drainage system that allows the fluid or air to be evacuated from the pleural cavity. This procedure provides immediate relief from symptoms such as chest pain and shortness of breath and helps re-expand the collapsed lung. Chest tube insertion is often guided by imaging techniques, such as ultrasound or CT, to ensure accurate placement.
Pleurodesis
Pleurodesis is a procedure used to prevent recurrent pleural effusions or pneumothorax by causing the pleurae to adhere together. This can be achieved through chemical or mechanical means. Chemical pleurodesis involves instilling a sclerosing agent, such as talc, doxycycline, or bleomycin, into the pleural space. These agents induce an inflammatory reaction that leads to fibrosis and adhesion of the pleural layers, effectively obliterating the pleural cavity and preventing fluid or air accumulation. Mechanical pleurodesis involves abrasion of the pleural surfaces during surgery to achieve the same result. Pleurodesis is particularly useful for patients with malignant pleural effusions or recurrent spontaneous pneumothorax.
Video-Assisted Thoracoscopic Surgery (VATS)
Video-assisted thoracoscopic Surgery (VATS) is a minimally invasive surgical technique used for diagnosing and treating various pleural diseases. During VATS, a thoracoscope (a small camera) and surgical instruments are inserted through small incisions in the chest wall. This allows the surgeon to visualize the pleural cavity and perform procedures such as biopsy, drainage of pleural effusions, decortication (removal of thickened pleural tissue), and pleurodesis.
VATS offers several advantages over traditional open surgery, including smaller incisions, reduced pain, shorter hospital stays, and faster recovery times. It is an effective and versatile approach for managing pleural conditions while minimizing patient morbidity.
The treatment and management of pleural disorders involve a combination of medical therapies and surgical interventions tailored to the underlying cause and severity of the condition. Antibiotics, anti-inflammatory medications, and diuretics play vital roles in addressing infections, reducing inflammation, and managing fluid accumulation. Surgical procedures such as chest tube insertion, pleurodesis, and VATS provide definitive solutions for drainage, preventing recurrence, and treating complex pleural diseases.
A comprehensive and individualized approach ensures optimal patient outcomes and improves the quality of life for those affected by pleural disorders. Advances in medical technology and surgical techniques continue to enhance our ability to diagnose, treat, and manage pleural conditions effectively.
Research and Advances in Pleural Medicine
Biomarkers for Pleural Diseases
Research is ongoing to identify specific biomarkers in pleural fluid that can aid in the diagnosis of pleural malignancies, infections, and other conditions. These biomarkers can provide non-invasive, rapid, and accurate diagnostic information.
Advances in Imaging Techniques
New imaging modalities, such as magnetic resonance imaging (MRI) and positron emission tomography (PET) scans, are being explored for better characterization of pleural diseases. These advanced techniques can provide more precise information about pleural anatomy and pathology.
Immunotherapy and Targeted Therapy
Immunotherapy and targeted therapies are being investigated for the treatment of pleural malignancies, such as mesothelioma. These therapies aim to enhance the immune system’s ability to fight cancer cells and target specific molecular pathways involved in tumor growth.
Conclusion
The inner serosa membrane, or visceral pleura, plays a crucial role in the respiratory system, providing protection, facilitating lung movement, and maintaining the necessary pressure dynamics for breathing. Understanding its anatomy, function, and associated clinical conditions is essential for diagnosing and managing pleural diseases effectively. Ongoing research and advances in medical technology continue to enhance our knowledge and treatment options for pleural disorders, improving patient outcomes and quality of life.
Frequently Asked Questions (FAQs)
What is the pleura, and what are its main functions?
The pleura is a double-layered serous membrane that envelops the lungs and lines the thoracic cavity. Its primary functions include protecting the lungs from infections and physical injuries, facilitating smooth lung movement during respiration by providing lubrication and maintaining a negative pressure within the pleural cavity to keep the lungs expanded.
What are the common symptoms of pleural effusion?
Pleural effusion, which is the accumulation of excess fluid in the pleural cavity, commonly presents with symptoms such as chest pain, shortness of breath, cough, and reduced lung function. These symptoms occur because the excess fluid compresses the lung and limits its expansion during breathing.
How is pleural effusion diagnosed?
Pleural effusion is typically diagnosed using imaging studies such as chest X-rays, CT scans, and ultrasounds. These imaging techniques help visualize the fluid accumulation. Additionally, thoracentesis, a procedure to aspirate pleural fluid for laboratory analysis, can provide information on the cause of the effusion by examining the fluid’s biochemical, cytological, and microbiological properties.
What is pleurodesis, and when is it used?
Pleurodesis is a procedure used to adhere the pleurae together to prevent recurrent pleural effusions or pneumothorax. This can be done chemically, using sclerosing agents like talc or doxycycline, or mechanically, through surgical abrasion. Pleurodesis is commonly used for patients with malignant pleural effusions or recurrent spontaneous pneumothorax to prevent the reaccumulation of fluid or air in the pleural cavity.
How have imaging techniques advanced in diagnosing pleural diseases?
Recent advances in imaging techniques, such as MRI and PET scans, have significantly improved the diagnosis and characterization of pleural diseases. MRI offers superior soft tissue contrast, making it ideal for assessing pleural thickening and tumors. PET scans provide functional imaging to detect metabolic activity in pleural malignancies, helping in the diagnosis, staging, and monitoring of treatment response.
What are the latest treatments for pleural malignancies?
The latest treatments for pleural malignancies include immunotherapy and targeted therapy. Immunotherapy, using drugs like checkpoint inhibitors, enhances the immune system’s ability to fight cancer cells. Targeted therapy focuses on specific molecular pathways crucial for cancer cell survival and proliferation. Combination therapies and gene therapy are also being explored to improve treatment efficacy and patient outcomes.